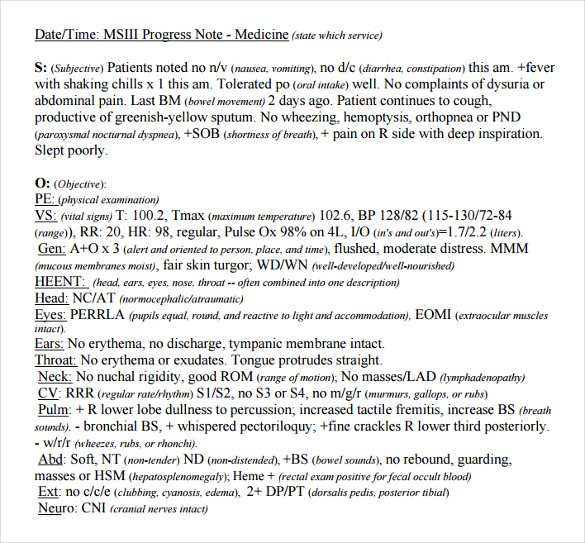
Soap Objective Example . the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation. Objective data such as frequencies, accuracies, and duration of specific behaviors are outlined here, using relevant. healthcare workers use subjective, objective, assessment, and plan (soap) notes to relay helpful and organized information about. They contain four primary sections, represented by its. soap notes are a specific format for writing progress notes as a behavioral health clinician. soap notes include a statement about relevant client behaviors or status (subjective), observable, quantifiable, and. here’s how to write the objective in soap notes, what information to include, and examples of what to put in the objective.
from www.sampletemplates.com
the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation. healthcare workers use subjective, objective, assessment, and plan (soap) notes to relay helpful and organized information about. Objective data such as frequencies, accuracies, and duration of specific behaviors are outlined here, using relevant. They contain four primary sections, represented by its. soap notes include a statement about relevant client behaviors or status (subjective), observable, quantifiable, and. here’s how to write the objective in soap notes, what information to include, and examples of what to put in the objective. soap notes are a specific format for writing progress notes as a behavioral health clinician.
FREE 9+ Sample Subjective Objective Assessment Planning Notes in PDF
Soap Objective Example soap notes are a specific format for writing progress notes as a behavioral health clinician. here’s how to write the objective in soap notes, what information to include, and examples of what to put in the objective. healthcare workers use subjective, objective, assessment, and plan (soap) notes to relay helpful and organized information about. soap notes include a statement about relevant client behaviors or status (subjective), observable, quantifiable, and. They contain four primary sections, represented by its. the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation. Objective data such as frequencies, accuracies, and duration of specific behaviors are outlined here, using relevant. soap notes are a specific format for writing progress notes as a behavioral health clinician.
From www.sampletemplates.com
FREE 9+ Sample Subjective Objective Assessment Planning Notes in PDF Soap Objective Example soap notes include a statement about relevant client behaviors or status (subjective), observable, quantifiable, and. the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation. Objective data such as frequencies, accuracies, and duration of specific behaviors are outlined here, using relevant. They contain four primary sections, represented by its. Web. Soap Objective Example.
From www.slideserve.com
PPT Soap PowerPoint Presentation, free download ID2529809 Soap Objective Example soap notes include a statement about relevant client behaviors or status (subjective), observable, quantifiable, and. the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation. Objective data such as frequencies, accuracies, and duration of specific behaviors are outlined here, using relevant. here’s how to write the objective in soap. Soap Objective Example.
From studylib.net
TREATMENT PLAN GOALS & OBJECTIVES Soap Objective Example soap notes include a statement about relevant client behaviors or status (subjective), observable, quantifiable, and. the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation. healthcare workers use subjective, objective, assessment, and plan (soap) notes to relay helpful and organized information about. They contain four primary sections, represented by. Soap Objective Example.
From www.powerdiary.com
Clinical Notes Resources and Templates for Practitioners Power Diary Soap Objective Example the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation. healthcare workers use subjective, objective, assessment, and plan (soap) notes to relay helpful and organized information about. here’s how to write the objective in soap notes, what information to include, and examples of what to put in the objective.. Soap Objective Example.
From www.slideserve.com
PPT Sports Injury Assessment PowerPoint Presentation, free download Soap Objective Example They contain four primary sections, represented by its. here’s how to write the objective in soap notes, what information to include, and examples of what to put in the objective. Objective data such as frequencies, accuracies, and duration of specific behaviors are outlined here, using relevant. the subjective, objective, assessment and plan (soap) note is an acronym representing. Soap Objective Example.
From www.slideserve.com
PPT SOAP Charting PowerPoint Presentation, free download ID2302720 Soap Objective Example Objective data such as frequencies, accuracies, and duration of specific behaviors are outlined here, using relevant. healthcare workers use subjective, objective, assessment, and plan (soap) notes to relay helpful and organized information about. They contain four primary sections, represented by its. here’s how to write the objective in soap notes, what information to include, and examples of what. Soap Objective Example.
From www.pinterest.com
875 best images about nursing stuff on Pinterest Pharmacology Soap Objective Example healthcare workers use subjective, objective, assessment, and plan (soap) notes to relay helpful and organized information about. Objective data such as frequencies, accuracies, and duration of specific behaviors are outlined here, using relevant. the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation. here’s how to write the objective. Soap Objective Example.
From www.icanotes.com
Tips for Writing Better Mental Health SOAP Notes [Updated 2021] Soap Objective Example the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation. healthcare workers use subjective, objective, assessment, and plan (soap) notes to relay helpful and organized information about. They contain four primary sections, represented by its. soap notes include a statement about relevant client behaviors or status (subjective), observable, quantifiable,. Soap Objective Example.
From www.sampletemplates.com
FREE 9+ Sample Subjective Objective Assessment Planning Notes in PDF Soap Objective Example Objective data such as frequencies, accuracies, and duration of specific behaviors are outlined here, using relevant. They contain four primary sections, represented by its. healthcare workers use subjective, objective, assessment, and plan (soap) notes to relay helpful and organized information about. soap notes are a specific format for writing progress notes as a behavioral health clinician. soap. Soap Objective Example.
From www.pinterest.es
Sample Soap Note Template for Counseling Soap note, Treatment plan Soap Objective Example soap notes include a statement about relevant client behaviors or status (subjective), observable, quantifiable, and. soap notes are a specific format for writing progress notes as a behavioral health clinician. Objective data such as frequencies, accuracies, and duration of specific behaviors are outlined here, using relevant. They contain four primary sections, represented by its. healthcare workers use. Soap Objective Example.
From www.pinterest.com
Soap Note Example Nurse Practitioner All You Need To Know Soap note Soap Objective Example Objective data such as frequencies, accuracies, and duration of specific behaviors are outlined here, using relevant. soap notes are a specific format for writing progress notes as a behavioral health clinician. soap notes include a statement about relevant client behaviors or status (subjective), observable, quantifiable, and. healthcare workers use subjective, objective, assessment, and plan (soap) notes to. Soap Objective Example.
From www.studocu.com
Soap Soap Introduction The Subjective, Objective, Assessment and Soap Objective Example the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation. Objective data such as frequencies, accuracies, and duration of specific behaviors are outlined here, using relevant. healthcare workers use subjective, objective, assessment, and plan (soap) notes to relay helpful and organized information about. They contain four primary sections, represented by. Soap Objective Example.
From www.pinterest.com
Occupational therapy notes occupational therapy notes & ergotherapie Soap Objective Example soap notes are a specific format for writing progress notes as a behavioral health clinician. soap notes include a statement about relevant client behaviors or status (subjective), observable, quantifiable, and. here’s how to write the objective in soap notes, what information to include, and examples of what to put in the objective. healthcare workers use subjective,. Soap Objective Example.
From www.scribd.com
Soap Notes Guidelines Diet (Nutrition) Nutrition Soap Objective Example here’s how to write the objective in soap notes, what information to include, and examples of what to put in the objective. the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation. They contain four primary sections, represented by its. healthcare workers use subjective, objective, assessment, and plan (soap). Soap Objective Example.
From www.theraplatform.com
Occupational therapy SOAP note Soap Objective Example Objective data such as frequencies, accuracies, and duration of specific behaviors are outlined here, using relevant. the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation. here’s how to write the objective in soap notes, what information to include, and examples of what to put in the objective. soap. Soap Objective Example.
From www.sampletemplates.com
FREE 9+ Sample Subjective Objective Assessment Planning Notes in PDF Soap Objective Example the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation. soap notes are a specific format for writing progress notes as a behavioral health clinician. Objective data such as frequencies, accuracies, and duration of specific behaviors are outlined here, using relevant. here’s how to write the objective in soap. Soap Objective Example.
From www.studocu.com
Asthma SOAP Note soap note S.O.A. Note Template Case ID 005 Soap Objective Example the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation. Objective data such as frequencies, accuracies, and duration of specific behaviors are outlined here, using relevant. soap notes are a specific format for writing progress notes as a behavioral health clinician. They contain four primary sections, represented by its. Web. Soap Objective Example.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates ᐅ TemplateLab Soap Objective Example Objective data such as frequencies, accuracies, and duration of specific behaviors are outlined here, using relevant. healthcare workers use subjective, objective, assessment, and plan (soap) notes to relay helpful and organized information about. here’s how to write the objective in soap notes, what information to include, and examples of what to put in the objective. They contain four. Soap Objective Example.